This fact box will help you weigh the benefits of harms of immediate induction of labor for hypertensive disorders from the 34thweek of pregnancy. The information and numbers in this fact box represent no final evaluation. They are based on the best scientific evidence currently available.
This fact box was developed by the Harding Center for Risk Literacy.
Elevated blood pressure is defined as a systolic value of 140 mmHg (millimeters of mercury) or a diastolic value of 90 mmHg. Values of 120/80 mmHg are considered optimal blood pressure. The systolic value indicates the pressure in the vessels when the heart contracts. The diastolic value measures the vascular pressure when the heart muscle relaxes.
If blood pressure is permanently elevated, this puts strain on the blood vessels and increases the risk of secondary diseases (e.g., heart attack, kidney dysfunction, and stroke) and premature death [1].
High blood pressure can occur in completely healthy women during pregnancy. The causes of this are not fully understood [2].
High blood pressure during pregnancy occurs in about 6–8 per 100 pregnancies in Europe and can lead to various complications, such as premature detachment of the placenta or premature birth. In severe cases, permanently high blood pressure can lead to preeclampsia or HELLP syndrome. Depending on both the point in the pregnancy at which HELLP syndrome occurs and the health care available, it can lead to death in about 1–25 of every 100 affected mothers and in about 7–34 deaths of their newborns worldwide [2, 3, 4].
Preeclampsia
Preeclampsia is a pregnancy disorder that occurs in about 2 out of every 100 pregnancies in European countries [4].
In preeclampsia, blood pressure rises, more protein is excreted in the urine, and water retention (edema) occurs in the body. Untreated preeclampsia can harm both mother and baby [3].
A severe form of preeclampsia is eclampsia, in which the mother experiences stiffening and fitful seizures. Eclampsia may be recognized by upper abdominal shivering, nausea, vomiting, eye flutter, persistent headache, and increased reflexes (i.e. reflexes can be triggered more easily and may be more severe) [5].
A severe side effect of preeclampsia is HELLP syndrome.
HELLP syndrome
HELLP stands for:
(H) hemolysis (degradation of red blood cells)
(EL) elevated liver enzymes
(LP) low platelets (thrombocytopenia)
Persistent upper abdominal pain usually occurs in HELLP syndrome [5].
In many cases, the hypertension and mild preeclampsia resolve on their own within the first 32 weeks of pregnancy. If the conditions persist until the 34th week of pregnancy, a decision must be made on the appropriate course of clinical action [3]: immediate induction of labor or “wait and see” (expectant management).
Blood pressure is measured as part of routine maternity care. If significantly elevated blood pressure is detected repeatedly, further tests (e.g., urine and blood tests) are performed to rule out other causes of high blood pressure [3].
If the blood pressure rises permanently to or above 150/100 mmHg, inpatient monitoring in hospital is required [3].
There are two treatment options for high blood pressure with or without increased protein excretion in the urine (preeclampsia) from the 34th week of pregnancy. One option is to induce labor immediately. The other is to wait for birth under regular medical monitoring. Medical care can be provided on an outpatient or inpatient basis, during which blood pressure is measured and protein levels in the urine are determined. In addition, the pregnant woman can be examined for preeclampsia symptoms, and the baby can be examined with regard to its movements and heart rate.
In this review, births were induced by amniotomy (opening of the amniotic sac) or by administration of oxytocin (a contraction drug). If necessary, prostaglandins were administered to help open the cervix [3].
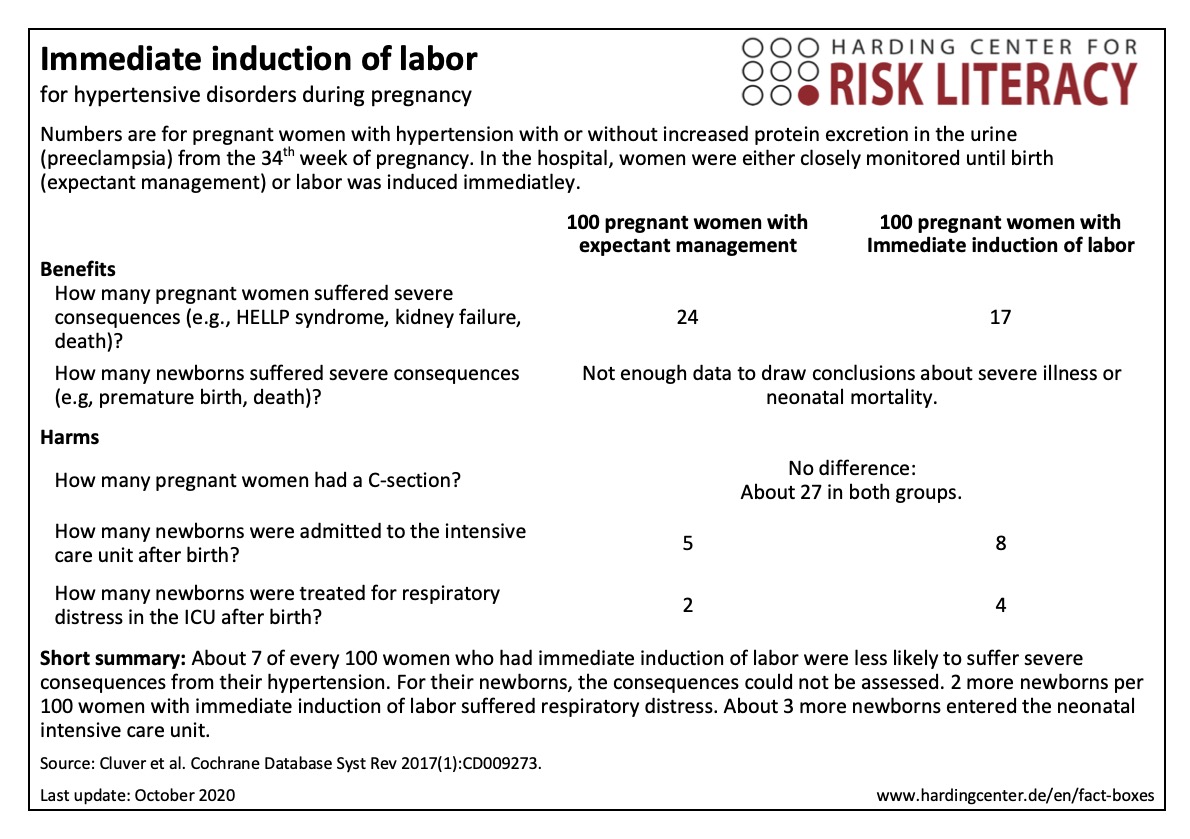
The fact box compares two treatment options for hypertensive disorders during pregnancy (expectant management and immediate induction of labor) regarding their benefits and harms for both mother and newborn.
The table may be read as follows:
24 out of every 100 women with expectant management and 17 out of every 100 women with immediate induction of labor suffered from severe consequences (e.g., HELLP syndrome, kidney failure, death) of their pregnancy-related hypertensive disorder. This means that in 7 out of every 100 women severe consequences were prevented by the immediate induction of labor.
The numbers in the fact box are rounded. They are based on five studies with 1,819 participants [1].
| Frauen ab 34 SSW mit Bluthochdruck im Alter von 18-50 Jahren | Frauen ab 34 SSW mit Bluthochdruck unter 18 Jahren | Andere Frauen |
| X | ? | - |
Erklärung der Symbole: X = für diese Personen gelten die Zahlen in der Faktenbox; (X) = auf diese Personen lassen sich die Zahlen unter Vorbehalt anwenden (in solchen Fällen ist eine Rücksprache mit ärztlichem Personal empfehlenswert); - = für diese Personen gelten die Zahlen nicht; ? = es ist unbekannt, ob die Zahlen für diese Personen gelten
The evidence was assessed by the authors of the review included. According to their assessment, the evidence is, depending on the benefit or harm in question, of non-assessable to high quality.
The results on severe consequences for newborns could not be assessed. There were not enough data to make a statement about severe consequences for newborns.
It is very unlikely that further research will change the results on severe consequences (e.g., HELLP syndrome, kidney failure, death) for mothers (high evidence).
The results on the number of C-sections might be changed by further research (moderate evidence).
An assessment of the evidence on respiratory distress syndrome in newborns and the number of newborns treated in a neonatal intensive care unit was not carried out by the authors of the review.
- October 2020 (update of the research, no new evidence; update of the accompanying text)
- February 2017 (development)
Information within the fact box was obtained from the following sources:
[1] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Bluthochdruck 2019. Abrufbar unter: https://www.gesundheitsinformation.de/bluthochdruck-hypertonie.2083.de.html (23.10.2020).
[2] Haram K, Svendsen E, Abildgaard U. The HELLP syndrome: Clinical issues and management. A Review. BMC Pregnancy and Childbirth 2009, 9:8. doi: 10.1186/1471-2393-9-8.
[3] Cluver C, Novikova N, Koopmans CM, et al. Planned early delivery versus expectant management for hypertensive disorders from 34 weeks gestation to term. Cochrane Database of Systematic Reviews 2017(1). doi: 10.1002/14651858.CD009273.
[4] Deutsche Gesellschaft für Gynäkologie und Geburtshilfe e.V. (DGGG), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). S2k-Leitlinie Hypertensive Schwangerschaftserkrankungen: Diagnostik und Therapie (AWMF-Registrierungsnummer: 015/018, März 2019).
[5] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Schwangerschafts-diabetes 2020. Abrufbar unter: www.gesundheitsinformation.de/schwangerschaftsdiabetes.2108.de.html (23.10.2020).
