This fact box will help you to weigh the benefits and harms of imaging tests for low back pain. The information and numbers are based on the best scientific evidence currently available.
This fact box was developed by the Harding Center for Risk Literacy.
Low back pain refers to pain in the lower back (between the hips and rib cage). The pain can radiate to the gluteal muscles, legs, and feet [2]. It is estimated that about 85 % of the German population suffer from back pain at least once during their lifetime. About 76 % experience back pain at least once a year [3].
The causes of low back pain are often unclear. If no distinct cause can be determined, it is called non-specific low back pain. This can be caused by muscle tension and stiffness due to weak core muscles, poor posture, or muscle or joint strain, as well as by psychosocial factors such as stress, anxiety, and depression. Specific low back pain refers to pain caused by mechanical problems such as fractures, herniated discs, spinal stenosis, and spondylitis. Other specific causes could be chronic diseases, including osteoporosis, cancer, and organic diseases (e.g. kidney stones) [2, 4, 5].
Low back pain can be classified as either acute when it lasts less than six weeks or as chronic when it lasts longer than 12 weeks [3].
Different imaging procedures such as X-rays, computed tomography scans (CT scans), and magnetic resonance imaging (MRI) are used to determine the causes of low back pain.
X-rays depict bone structures and are used to diagnose fractures, postural defects, and deformities.
CT scans utilize a 3D X-ray technique that shows calcified ligaments, tendons, and spinal discs in addition to bones and joints.
MRIs can produce detailed images of soft tissue and bone marrow [4]. Therefore, it is often used to clarify typical the symptoms of herniated discs.
Unlike X-rays and CT scans, MRIs do not expose patients to damaging ionizing radiation because they use magnet fields and radio signals instead [4]. Ionizing radiation may cause changes to DNA, which increase the risk of cancer.
Patients who experience acute or recurring low back pain without any specific indications of the source of pain are advised to refrain from imaging tests by the Nationalen VersorgungsLeitlinie (NVL) Nicht–spezifischer Kreuzschmerz (”National Disease Management Guideline Low Back Pain”).
If low back pain persistently limits physical activity or grows worse after four to six weeks, imaging may be considered.
Imaging tests can be useful if serious conditions (“red flags”) are suspected. Red flags are indicators for cancer, nerve damage, herniated discs, inflammations of the spine, and bone fractures. In these cases, MRI is considered the best diagnostic procedure because of its accuracy [2].
Advice and education about lifestyle-related causes should be emphasized for patients with acute and non-specific low back pain. This includes measures for increasing physical activity and self-management, e.g. coping mechanisms for stress.
Accompanying treatment with drugs (painkillers) or without drugs (e.g. physiotherapy, manual therapy, acupuncture) can help to relieve pain [2].
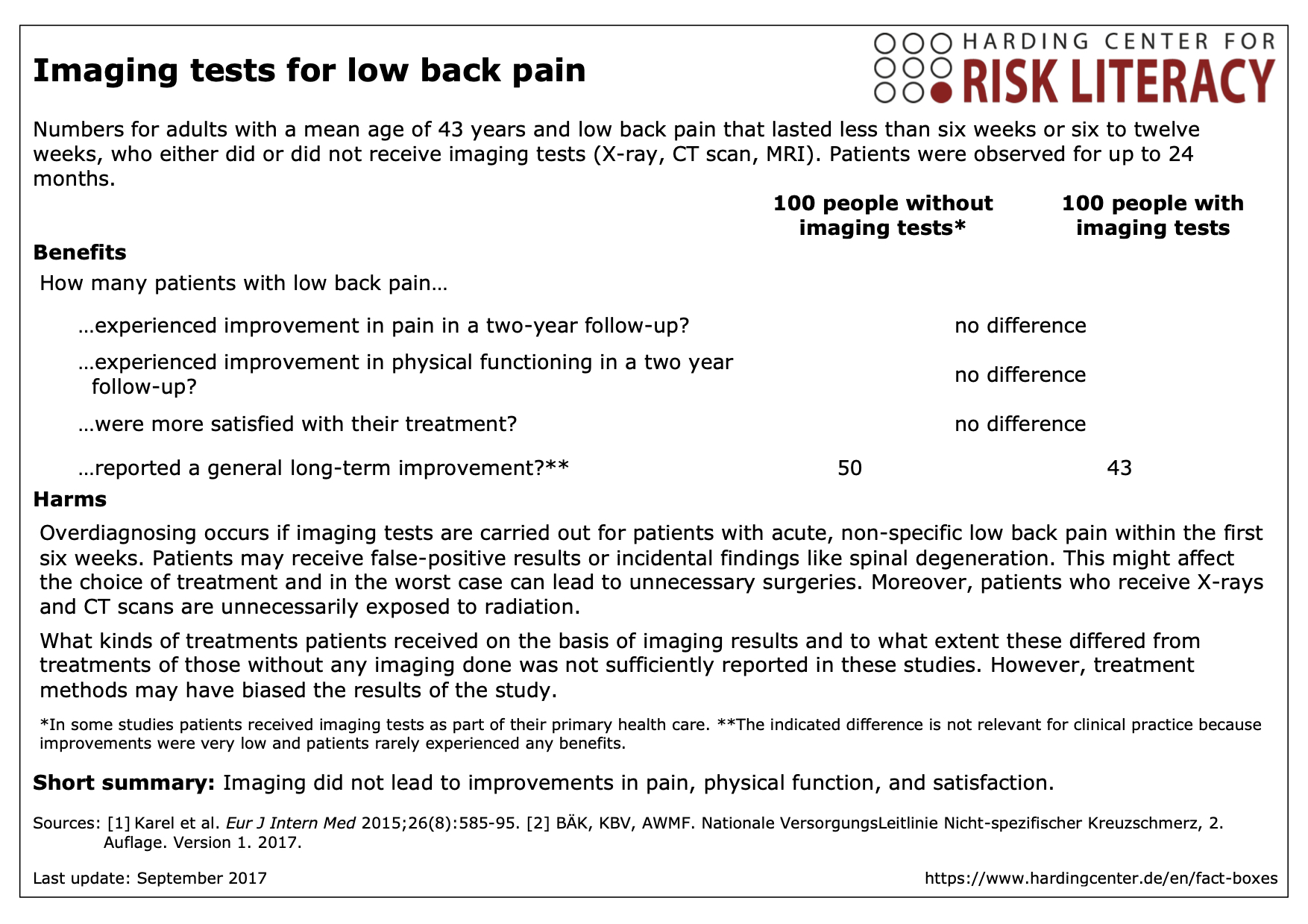
The fact box shows the benefits and harms of imaging tests for patients with low back pain who were observed for up to 24 months compared to patients who did not receive any imaging.
The table may be read as follows:
There was no difference in outcomes in terms of pain, physical functioning, and satisfaction in patients with low back pain. 50 out of every 100 patients without imaging reported long-term overall improvement. 43 out of every 100 patients with imaging reported the same effect.
The numbers in the fact box are rounded. The data on benefits were reported in seven studies with about 2,000 participants [1].
Imaging procedures in the studies included X-rays, CT scans, and MRIs. X-rays were most commonly used (in four studies), followed by MRIs (three studies) and CT scans (one study).
After imaging, some specific causes of low back pain can be ruled out, leading by exclusion to the diagnosis of non-specific low back pain [6]. But there is also a chance of incidental findings such as spinal degeneration, which might influence the choice of treatment. However, spinal degeneration can occur in people both with and without low back pain [4]. Therefore, a degeneration found during imaging is not necessarily the cause of existing pain. This can confuse patients and prolong their recovery process.
There was no difference in quality of life between patients with and without imaging tests.
Overall, the evidence is of low to moderate quality: Further research is likely to have an important impact on some findings (those of moderate quality of evidence), while other findings are very likely to be changed in the course of further research (low quality of evidence).
- September 2017 (last update)
Information within the fact box was obtained from the following sources:
[1] Karel YH, Verkerk K, Endenburg S, et al. Effect of routine diagnostic imaging for patients with musculoskeletal disorders: A meta-analysis. Eur J Intern Med 2015;26(8):585-95. doi: 10.1016/j.ejim.2015.06.018
[2] Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale VersorgungsLeitlinie Nicht-spezifischer Kreuzschmerz – Langfassung, 2. Auflage. Version 1. 2017. DOI: 10.6101/AZQ/000353. www.kreuzschmerz.versorgungsleitlinien.de
[3] Schmidt CO, Raspe H, Pfingsten M, et al. Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine 2007;32(18):2005-11. doi: 10.1097/BRS.0b013e318133fad8
[4] Hansen BB, Hansen P, Carrino JA, et al. Imaging in mechanical back pain: Anything new? Best Pract Res Clin Rheumatol2016;30(4):766-85. doi: http://dx.doi.org/10.1016/j.berh.2016.08.008
[5] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Rücken- und Kreuzschmerzen 2015 [Available from: www.gesundheitsinformation.de/kreuzschmerzen.2378.de.html.
[6] Linder R, Horenkamp-Sonntag D, Engel S, et al. Überdiagnostik mit Bildgebung bei Rückenschmerzen. Dtsch Med Wochenschr 2016;141(10):e96-e103. doi: 10.1055/s-0042-101467
Documentation on how the numbers in the fact box were determined is available on request.
