This fact box will help you to weigh the benefits and harms of ultrasound screenings for the early detection of ovarian cancer. The fact box is for women considering ultrasound for early ovarian cancer detection without a health reason (no symptoms related to ovarian cancer). The information and numbers in this fact box represent no final evaluation. They are based on the best scientific evidence currently available.
The fact box was developed by the Harding Center for Risk Literacy.
The ovaries are part of the female reproductive organs. Malignant or benign cell changes in one of the tissues of the ovaries can lead to the growth of a tumor. If there is an increased and uncontrolled cell growth, which causes the tumor to spread into healthy neighboring tissue or to detach itself from the cluster of tumors, this is called a malignant tumor or ovarian cancer (ovarian carcinoma). Ovarian cancer often goes unnoticed in the early stages because there are usually no symptoms. As the tumor grows in size, abdominal pain, bloating, constipation and changes in digestion may occur. More frequent urination, vague weight loss, and an increase in abdominal girth may also be indications [4].
About 13 out of every 1,000 women will develop ovarian cancer during their lifetime [5], 10 of whom will die from it [6]. Women who receive a diagnosis of ovarian cancer are 68 years of age on average. Increasing age is a risk factor. In addition, ovarian cancer develops more frequently in women whose first-degree relatives (mother, sister) have had breast or ovarian cancer. Obesity, childlessness, and infertility may also increase the risk of developing ovarian cancer [5].
For early cancer detection, women are offered an ultrasound screening of the ovaries.
Early detection examinations (also called screening) are aimed at people who have no symptoms in relation to the disease in question (in this case ovarian cancer). The purpose of the ultrasound examination of the ovaries by a gynecologist is to detect and treat ovarian cancer at an earlier stage [5].
Ultrasound screenings can be used to visualize organs and blood vessels within the body. During this process, the emitted sound waves are reflected by the different tissues to varying degrees, thus creating an image. Depending on the body part and tissue, the doctor may have to apply a little more pressure to get a better image of the organ or vessel being examined. However, pain should not occur during the examination. In contrast to an X-ray examination, there is no exposure to radiation during an ultrasound [7].
For an ultrasound examination of the ovaries, the ultrasound probe is inserted into the vagina (vaginal ultrasound) to obtain the most accurate image of the ovaries and to detect possible tissue changes. This can be uncomfortable, but is not associated with pain [6].
If a tumor is suspected, further imaging examinations are possible, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to obtain a more accurate image and to assess the extent of the changes in the tissue [5]. Currently, there is no scientific evidence that the course of the disease can be improved or that the risk of dying can be reduced through these procedures [4]. Ovarian cancer can only be reliably detected by surgery. In this case, the affected ovary is removed and examined microscopically to confirm or eliminate the suspected cancer [4; 5].
For early detection of ovarian cancer, many gynecologists in Germany offer ultrasound screening of the ovaries. This is often performed in the context of gynecological cancer screening. If ovarian cancer is suspected, i.e. if symptoms related to the disease appear, the costs of this examination are covered by one’s health insurance. If ovarian cancer is not suspected, this screening procedure is an individual health care service (IGeL) and must be paid for by the patients themselves [5].
Women over the age of 20 can have an annual cancer screening examination by their gynecologist. This includes, among other things, palpation of the lower abdomen and pelvic area and a smear test of cells from the cervix for the early detection of cervical cancer. Blood tests, such as testing for the tumor marker CA-125, are also offered occasionally [8].
The available studies do not show evidence of benefits for any of these screening tests. This means that these tests cannot determine whether ovarian cancer is in fact evident. Further examinations are necessary if cancer is suspected [9].
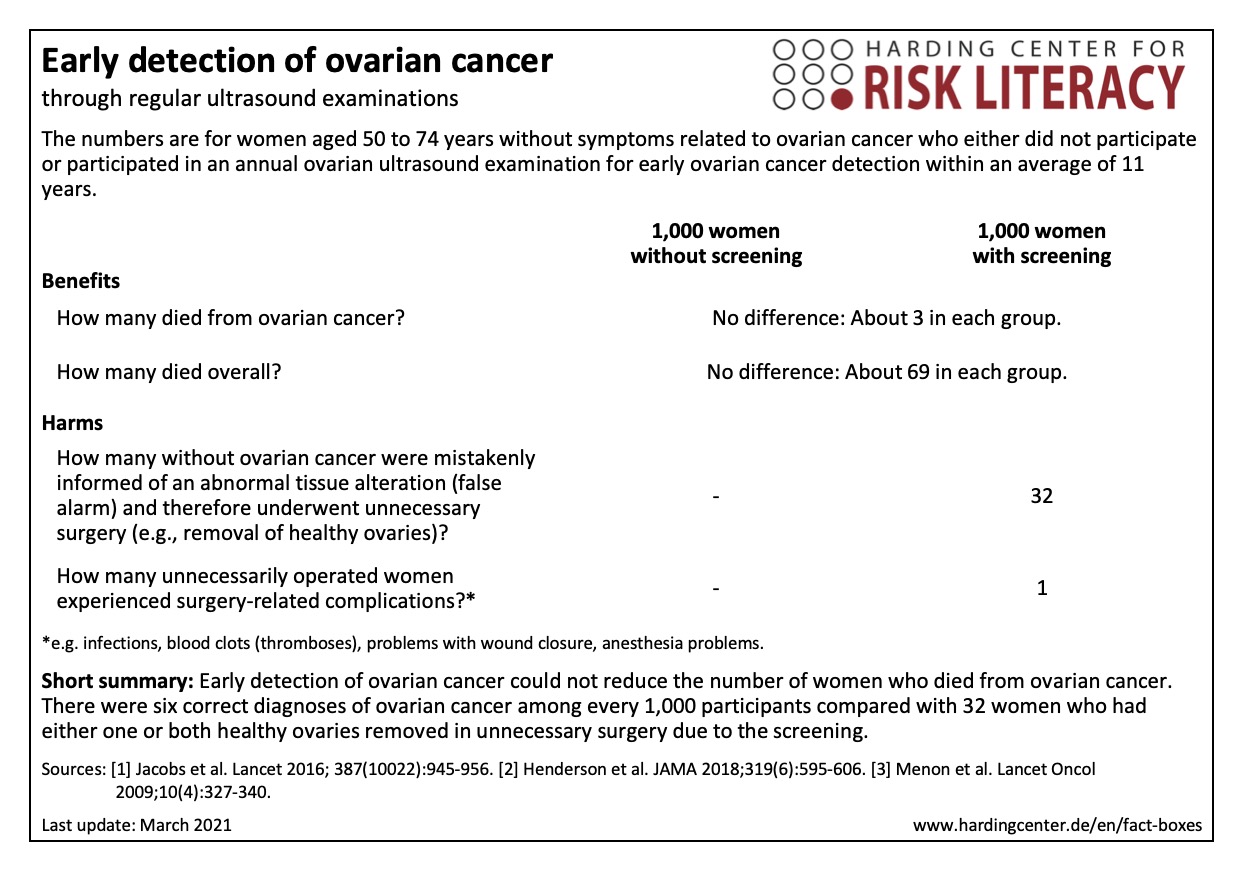
The fact box compares the benefits and harms of non-participation with those of participation in early detection of ovarian cancer.
The table may be read as follows:
About 3 out of every 1,000 women with or without early detection died from ovarian cancer within 11 years.
The numbers in the fact box are rounded. They are based on a large study with about 200,000 participants who underwent a nearly annual ultrasound examination of the ovaries for early detection of ovarian cancer for 7 to 14 years [1; 2].
In the interpretation of the ultrasound findings in the study, approximately one in five tumors was either missed by selected experts despite annual examinations or was too small to be detected at the time of the examination [3].
Additionally, the underlying study investigated the combined screening of ultrasound and blood testing for the tumor marker CA-125 in another study branch. Once again, the same number of women as for those without systematic screening by blood testing for CA-125 died from ovarian cancer over an average of 11 years. A reduction in ovarian cancer-specific mortality of 0 to 1 in every 1,000 women who had ultrasound examinations combined with blood testing for at least 7 to 14 years cannot be ruled out [1].
False alarms caused by ovarian cancer screening in women without symptoms and family history may lead to unnecessary surgical interventions as well as to unnecessary uncertainty and psychological distress for affected women [2].
The evidence was assessed by the authors of the review included. According to their assessment, the evidence is of overall high quality.
The results presented here are taken from one large study only. Because of the small number of new cases of ovarian cancer, very large studies are needed to determine whether the benefits of a screening program outweigh the harms, which include surgery and removal of the ovaries. In addition, a longer observation period is needed to conclusively assess the impact of screening on mortality and to draw conclusions regarding long-term efficacy [1; 2].
-
March 2021 (update of the research, no new evidence; update of the accompanying text)
-
June 2016 (development)
Information within the fact box was obtained from the following sources:
[1] Jacobs IJ, Menon U, Ryan A, et al. Ovarian cancer screening and mortality in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial. Lancet 2016;387(10022):945-56 doi: 10.1016/s0140-6736(15)01224-6.
[2] Henderson JT, Webber EM, Sawaya GF. Screening for Ovarian Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2018; 319(6):595-606.
[3] Menon U, Gentry-Maharaj A, Hallett R, et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncology 2009;10(4):327-40 doi: 10.1016/s1470-2045(09)70026-9.
[4] Leitlinienprogramm Onkologie der Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e. V., Deutschen Krebsgesellschaft e. V. und Stiftung Deutsche Krebshilfe (2020). Patientinnenleitlinie Eierstockkrebs. Abrufbar unter: www.leitlinienprogramm-onkologie.de/patientenleitlinien/eierstockkrebs/ (24.03.2021).
[5] IGeL-Monitor. Transvaginaler Ultraschall zur Früherkennung eines Ovarialkarzinoms (2020). Medizinischer Dienst des Spitzenverbandes Bund der Krankenkassen e.V. (MDS); Essen. Abrufbar unter: www.igel-monitor.de/igel-a-z/igel/show/ultraschall-der-eierstoecke-zur-krebsfrueherkennung.html?no_cache=1 (24.03.2021).
[6] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) (2021). Ultraschall zur Früherkennung von Eierstockkrebs. Abrufbar unter: www.gesundheitsinformation.de/ist-eine-ultraschalluntersuchung-zur-frueherkennung-von-eierstockkrebs-sinnvoll.html (23.03.2021).
[7] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) (2021). Wie funktioniert eine Ultraschalluntersuchung? Abrufbar unter: www.gesundheitsinformation.de/wie-funktioniert-eine-ultraschalluntersuchung.html (23.03.2021).
[8] IGeL Monitor. Ultraschall der Eierstöcke zur Krebsfrüherkennung (2020). Abrufbar unter: www.igel-monitor.de/igel-a-z/igel/show/ultraschall-der-eierstoecke-zur-krebsfrueherkennung.html?no_cache=1 (24.03.2021).
[9] Stiftung Gesundheitswissen (2021). Eierstockkrebs Früherkennung. Abrufbar unter: www.stiftung-gesundheitswissen.de/wissen/eierstockkrebs-frueherkennung/frueherkennung (23.03.2021).
